Hemorrhoids are a common disorder that can occur in both men and women at the age of around 20-50 years (Black & Hawks, 2009).
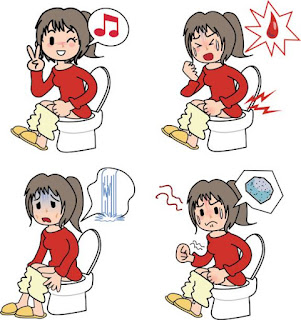
Patients with hemorrhoids will experience signs and symptoms including bleeding, painful prolapse (lumps) and sometimes itching in the rectum. Symptoms in the early stages of internal hemorrhoids are blood discharge that is bright red in color and is not accompanied by pain at the end of defecation. Meanwhile, the symptoms in the late stage are persistent prolapse and cannot enter again even though they are pushed manually (Syamsuhidayat & Joong, 2004).
The complications of hemorrhoids are acute bleeding, chronic bleeding and prolapsed incarceration. This can cause infection to sepsis and gangrene which causes a pungent odor (Prace, 2005; Fiona & Alexis, 2013).
Management of hemorrhoids can be done surgically and non-surgically. Non-surgical treatment includes sclerotherapy, Rubber Band Ligation (RBL), bipolar coagulation, infrared light (Lohsiriwat, 2012). The surgical management of hemorrhoids is hemorrhoidectomy. Hemorrhoidectomy is surgical removal of hemorrhoids by excision, namely by removing tissue that has varicose veins (widening) that occurs in the anal canal area (Jacobs, 2014).
Postoperative pain is caused by a mechanical stimulus due to tissue damage from surgical procedures, namely wounds (incisions), so that it will stimulate chemical mediators of pain (Potter & Perry, 2009). Post surgery makes the skin open and injured so that it stimulates pain impulses to the sensory nerves and is activated and transmitted to the posterior horn of the spinal cord. Afferent nerves will convey the perception of pain to the brain (Brazz, 2014).
Non-pharmacological pain management that nurses can do include providing skin stimulation, relaxation and distraction, massage, cold compresses, warm compresses, providing a comfortable position, acupuncture, hydrotherapy. Transcutaneous Electrical Stimulation Nerve Stimulation (TENS) is a type of skin stimulation (Demir, 2012). ). Cold compresses reduce prostaglandins that strengthen pain receptors, inhibit the inflammatory process and stimulate the release of endorphins.
Cold compress is a procedure of placing a cold object on the outside of the body. The physiological impact is vasoconstriction in blood vessels, reducing pain, and decreasing the activity of nerve endings in muscles. The use of cold compresses has been proven to relieve pain, cold therapy has an analgesic effect by slowing the speed of nerve conduction so that fewer pain impulses reach the brain (Eva, 2013).
The principle underlying the reduction of pain by cold compresses is that cold compresses work by stimulating painless receptors, cold compresses can reduce prostaglandins which strengthen the sensitivity of pain receptors (Saputra, et al, 2017). Cold compresses have a physiological effect, namely reducing the inflammatory response, reducing blood flow and reducing edema, reducing local pain (Ayang et al, 2016).